Rest Easy!
What to Know About Healthy Sleep + Sleep Apnea
“You can sleep when you’re dead.”
We understand it as a “you only live once” adage regarding being constantly on the go, but ironically, not getting enough sleep could affect your health to the point of risk factors for life-altering accidents and disease.
While you have likely heard about sleep apnea, one of the most talked about sleep disorders, Michael F. Maguire, MD, of Fox Valley Pulmonary Medicine says the most common is Sleep Insufficiency Syndrome. It simply encompasses not getting enough sleep. But a short definition doesn’t make it less harmful.
“It’s estimated that about 1 ⁄ 3 of Americans—100 million people—have excessive sleepiness… that becomes important for a variety of reasons,” he says. “Drowsy driving is the No. 1 non-alcohol related cause of traffic fatalities. Brain health, heart health and overall health is affected. The cost of health care is higher in patients who don’t get enough sleep.”
“A healthy body begins with healthy sleep,” Dr. Rahul Subbarayan of Ear, Nose and Throat Specialists of Wisconsin, adds. “Poor, restless and interrupted sleep results in lower energy throughout the day and impacts mental acuity.
“The impact on mental health should also not be ignored. Poor sleep can result in worsened anxiety and depression which compounds all these issues. Poor sleep has been linked to high blood pressure, diabetes, chronic kidney disease, heart attack, stroke, depression, anxiety and a whole host of other medical issues. Healthy sleep allows for good energy throughout the day which has the exact opposite effect of the above.”
What is “Healthy” Sleep?
“Healthy sleep clinically is going through the correct stages of sleep, in the correct order for the appropriate time. Sleep is on a cycle. We pass through lighter stages into deeper stages on an approximately 90–120-minute cycle. Any disruption to this cycle can impair sleep efficacy,” Dr. Subbarayan explains.

There are four phases of sleep: N1, N2, N3 and Rapid Eye Movement (REM) sleep. The former deeper sleep phases (N1-3), also considered the most restorative, typically happen in the first half of the night while REM tends to dominate the second half of the night, when people dream.
Recent studies have shown that a function of “flushing out” brain toxins happens when you get that deep, restorative sleep.
“It was recently worked out that there is a flushing system. The brain actually shrinks through N3 sleep,” Dr. Maguire says. “It may be in other parts but right now it’s pretty much isolated to the deepest part of sleep. And if you don’t get that deep sleep those toxins stay there.”
Understanding Sleep Apnea: Risk Factors + Treatment
“Sleep apnea is a syndrome of disrupted sleep. Essentially, when we fall asleep the muscles in our bodies relax. In some people, excessive relaxation or poor muscle tone in the back of the nose, back of the mouth and lower in the throat can obstruct airflow,” Dr. Subbarayan explains. “Disrupted airflow leads to snoring and impaired oxygen delivery throughout the body. This sends a signal to the brain that oxygen levels are low resulting in the brain waking the body up which disrupts the normal sleep cycle.”
“Two things happen: the oxygen level gets really low and over time, that beats up on the heart and brain, resulting in heart attacks and strokes,” Dr. Maguire adds. “The second thing that happens is that it disrupts the normal cycle of sleep at night. So instead of getting that deep, restorative sleep you’re constantly in the light phase of sleep.
“A lot of people with sleep apnea can feel sleepy the next day, and every day, because they never get that deep sleep,” Maguire says. “But there are other people with sleep apnea who say, ‘I feel fine, I wake up refreshed every day.’ That’s the broad spectrum of sleep apnea.”
What is a common denominator, he says, is the beating up of the brain and heart over time, and also the cognitive issues: concentration, memory, and the risk factor of dementia and Alzheimer’s disease.
Most people with sleep apnea get diagnosed because of a sleeping partner. Someone sees something and thinks something’s not right with their breathing. He suggests looking past the stereotypical snorting, choking and gasping for breath, particularly in women who may simply sound as if something isn’t quite right.
Sleep apnea does not discriminate between men and women, nor is it solely found in adults. It can also affect children. However, its treatment often helps symptoms of another common disorder.
“Kids with attention deficit disorder (ADHD), if you diagnose sleep apnea and get them treated—a tonsillectomy or CPAP—the ADHD either goes away or is amazingly improved,” Dr. Maguire says. “It really makes a big impact.”
“Breathing better doesn’t necessarily equate to sleeping better. Certainly, being able to breathe at night is important. If someone has trouble breathing through their nose or their mouth, this will delay sleep onset, which can throw off their natural sleep rhythm,” Dr. Subbarayan says.
“However, improving nasal or oral breathing alone without addressing the other complexities of the sleep cycle may not result in greatly improved sleep. A global look examining diet, lifestyle, stress levels, health issues and overall sleep hygiene in conjunction with anatomic assessment will provide greater overall impact.”
The most common treatment for sleep apnea is the CPAP machine, an air pressure device helping to hold the throat open so the air can flow more naturally.
“It can be used every night, all night,” Dr. Todd Meyer of Ear, Nose and Throat Specialists of Wisconsin, explains. “CPAP works best when the nasal airway is clear of anatomic obstruction or allergic related congestion.
“Another popular noninvasive treatment device which is worn at night and may be effective for certain patients with mild sleep apnea which helps to prevent airway collapse by holding the tongue and jaw forward is known as an oral appliance device which is optimized with a trained dental provider.”
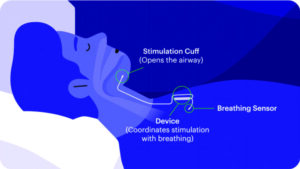
Inspire Therapy, another form of treatment, is typically reserved for those who don’t tolerate CPAP well and are still experiencing unpleasant symptoms of the sleep disorder.
“The hypoglossal nerve stimulator is essentially a pacemaker for the airway,” Dr. Subbarayan says. “It is a major surgery that requires insurance approval beforehand. The device senses when a person takes a breath and sends a signal to the nerve that controls the tongue to activate. This causes the tongue to stick out of the mouth opening up the airway.”
Healthy Sleep Advice + Sleep Study Options
Although likely not a surprise, healthy sleep not associated with diagnosed disorders begins with a scheduled routine.
“Try to go to bed at the same time and wake up at the same time,” Dr. Subbarayan suggests. “Avoid eating heavy meals within 1-2 hours of bedtime. Avoid screen time within 30 minutes to 1 hour before bedtime. Avoid caffeinated beverages or energy drinks within 6 hours of going to bed. Exercise and an active lifestyle will facilitate improved sleep as well.”
If all else fails and a sleep study is in order, you will likely be able to track your Zzzs at home.
“Over the last several years there has been an increased utilization of home sleep studies,” Dr. Meyer says. “These have been clinically validated for measuring sleep apnea and offer potential advantages over traditional in-lab sleep studies. They are more convenient, represent sleeping in a more natural home setting, less expensive and generally have a quicker turnaround.”











Leave a Comment